
Some of you may be aware that my 9 year old daughter was diagnosed with Type 1 Diabetes last year. To say that the time since has been an emotional roller coaster would be a gross understatement but thankfully she is doing great and adjusting really well.
While huge strides have been made in the treatment of T1D, one of the main things that the disease steals from you and your family is time and peace of mind. Finger pricks, injections, treating lows all occupy time away from living a regular life. What most people don't know is that with type 1, going low (i.e. blood sugar dropping) is far more dangerous that being high.
Type 1 Diabetes is a Family Disease
When you have type 1 diabetes, your body doesn't produce insulin so you have one choice: Add insulin via injections or die. Pretty much that simple.
The irony is that while we can't live without insulin due to its critical role of delivering energy (sugar) to our cells for normal brain and bodily functions, too much insulin can also kill you because it is incredibly efficient at delivering the sugar in your bloodstream to hungry cells (or fat storage if they’re well topped off). Without sugar (glucose to precise) your body, starting with your brain, literally shuts down. But too much sugar in the blood stream (which someone with T1D will always have without supplemental insulin) causes damage to organs and over time can lead to impaired eyesight, nerve damage and a host of other issues. So the key is to maintain a balance of external sugars (carbs) and insulin since your body (specifically, your pancreas) is unable to do so.
The problem is that we make crummy substitutes for doing the important work of the pancreas. The result is life that feels like your constantly walking a tightrope where one miscalculation in the amount of insulin administered could quickly turn into an emergency situation. Most families are very good at detecting the symptoms of hypoglycemia. Irritability, perspiration, nervous shakes and confusion are common indicators that someone with T1D is “going low” and so far my daughter has been really good about detecting these symptoms by staying in tune with her body and her feelings and being super responsible about her tests. We are extraordinarily fortunate to have an amazing care team including teachers, nurses and faculty at school, dance instructors, piano teachers and relatives who have learned the symptoms and can act in the event my daughter doesn’t realize she’s going low (sudden confusion is a common symptom). Maintaining this balance is especially frightening at night during sleep because it is possible to go low without recognizing the symptoms (the person is peacefully sleeping) and the family and care team are also asleep. Far too many children, young adults and grow ups have sadly died in their sleep because they didn’t realize they were going low and before they could medicate- as simple as drinking a juice box or eating a snack size pack of Skittles- its too late.
 The cure for parents of children with T1D is to set the alarm clock for 2 or 3 AM (a new routine in my home) and do a test to ensure that if she is low we can get her back up. 9.9 times out of 10 she is fine, right within range but we have had a couple of near lows. This is especially important on high exercise days like dance or running club because the body consumes more sugar (energy) during times of peak activity that can sometimes gradually bring sugar surplus down. In the event that someone with T1D is very high in the middle of the night (again, despite the utmost care, unlike the perfect pancreas and liver team, we can and will make mistakes in calculations) he or she must take insulin to bring the blood sugar down to non-damaging normal range, and that means a pretty awful, sleepless night with more finger pricks.
The cure for parents of children with T1D is to set the alarm clock for 2 or 3 AM (a new routine in my home) and do a test to ensure that if she is low we can get her back up. 9.9 times out of 10 she is fine, right within range but we have had a couple of near lows. This is especially important on high exercise days like dance or running club because the body consumes more sugar (energy) during times of peak activity that can sometimes gradually bring sugar surplus down. In the event that someone with T1D is very high in the middle of the night (again, despite the utmost care, unlike the perfect pancreas and liver team, we can and will make mistakes in calculations) he or she must take insulin to bring the blood sugar down to non-damaging normal range, and that means a pretty awful, sleepless night with more finger pricks.
As you can imagine, this is not fun for the someone living with T1D or their parents or caretakers, but the choice of giving up a full night’s sleep and bothering your little one with yet another finger prick is an easy trade off when the stakes are this high.
Fortunately, about twice a decade new innovation triumphs over the very high FDA bar to deliver new technology that makes living with Type 1 Diabetes a little easier. Examples include the advent of insulin pens with nano-needles over larger, clunky and more painful injections, home glucose testing kits over relying on highly inaccurate urine tests, or worse monthly visits to your doctor for lab work and insulin pumps that administer micro doses of  insulin and do a far better job of playing pancreas than we humans can.
insulin and do a far better job of playing pancreas than we humans can.
Continuous Glucose (Diabetes Nerdspeak for Blood Sugar) Monitoring
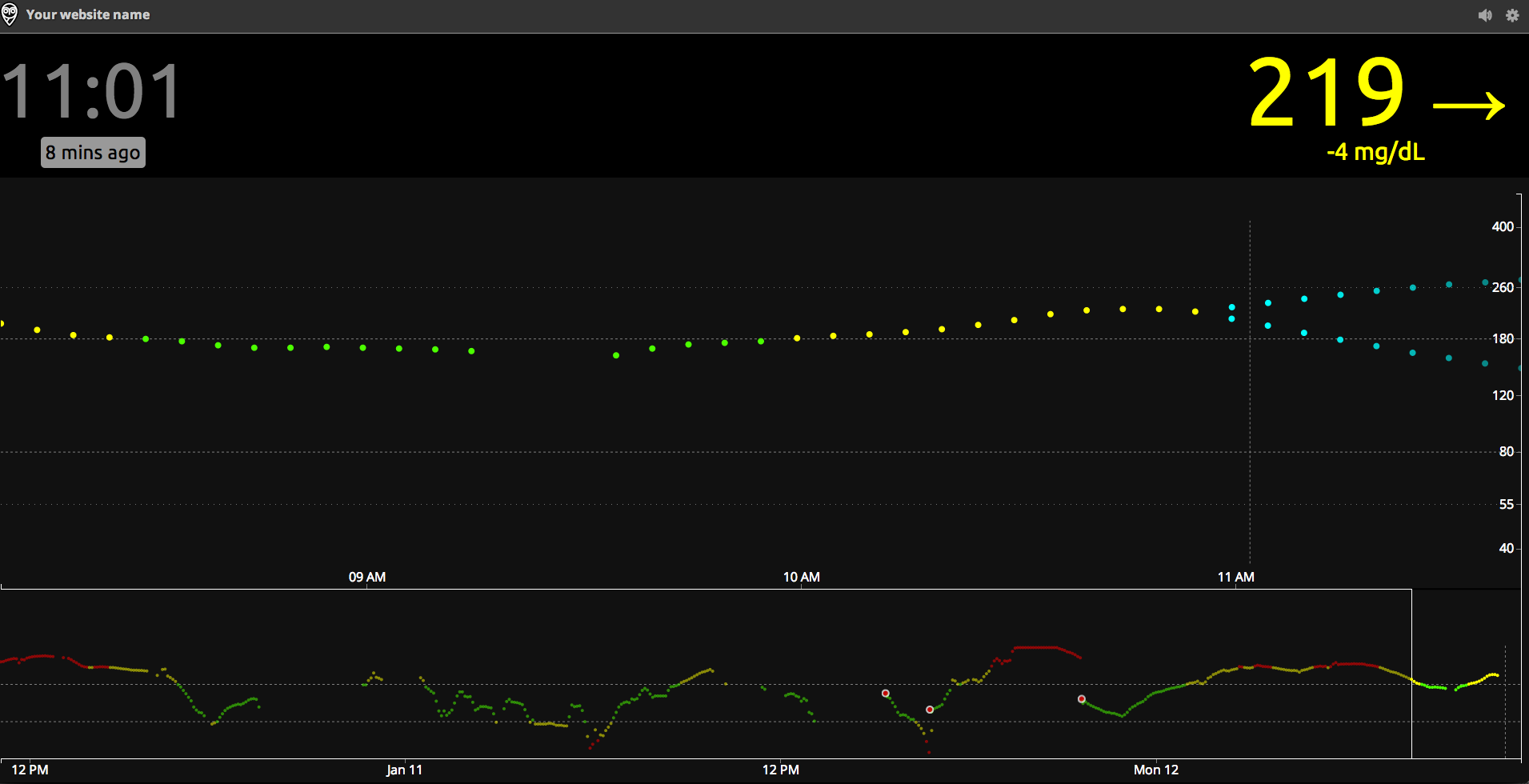
One such recent breakthrough has been in bringing continuous glucose monitoring (CGM) to the market. CGMs work by inserting a small needle exposed from a sensor about the size of a postage stamp (but much thicker) into the subcutaneous tissue and reading the current blood sugar in the blood stream at a given interval. The sensor then transmits the reading to a receiver about the size of a cell phone for display. While finger pricks are still required from time to time for calibration purposes, a CGM is a huge improvement to the quality of life of someone living with T1D and their care team because it not only provides the blood sugar information much more frequently, but given the frequency can also report on data trend. This is incredibly helpful in knowing if blood sugar is flat (good), rising (not good) or falling (really not good). For example, if a person with T1D is about to play in a tennis match and is within range but trending down, this data is enough to provide the insight to eat an apple or other healthy snack before the game. Likewise if after a celebratory pizza party blood sugar is still continuing to rise after administering X units of insulin, a corrective dose can be administered without missing it and going high for an afternoon.
So while CGMs are an amazing advancement in the treatment of T1D, alone they are not a panacea because while you still benefit from much more information much more frequently you still have to be awake to benefit from the data. Some devices (such as the Dexcom G4 Platinum) provide the ability to set hypo (low) and hyper (high) alarms which is a great step forward but snoozing through an alarm clock is something we’ve all experienced so still a risk. In addition, the information is isolated within the device and visible only to someone near the device.
CGM in the Cloud (The Nighscout Project)
This is where the work of amazing community that is the Nightscout Project comes in. The project is comprised of a 100% volunteer group of DIYers, all with day jobs who together are learning and sharing new ways to expose this critical data in a way that increases visibility and awareness for the entire care team. You can learn more about this great project here but in a nutshell, the project provides a reference architecture, guidance and code to stream this precious telemetry up to the Microsoft Azure cloud. The idea is that once the data is unshackled from the stand alone device, it can be shared openly. Imagine the peace of mind this brings to a parent who is wondering if his or her child got enough carbs before recess and with one click see a dashboard with live updates 5 minutes apart.
The dashboard running on Azure Websites.
Microsoft has committed to provide 1,500 families with six-month “Azure passes” to offset the cost of NightScout - See more at: http://diatribe.org/tech-giant-microsoft-teams-jdrf-champion-cloud-based-solutions-diabetes#sthash.xVBOG9g2.dpuf
That’s game changing in and of itself. But that’s really only the beginning. Once the data is landing on Azure, you are free to do with it what you want. This is where leveraging APIs for email or SMS come in. How nice would it be to get automatic updates anytime your child’s blood sugar is trending up or down, or be able to display the current blood sugar on a smart watch giving your child back just a little bit of dignity and freedom to just live life a little more care free like any kid should be able to?

Walking the T1D Tightrope: T1D in the Cloud
On Thursday, January 22nd, The JDRF Orange County Chapter, The Nightscout Project and Microsoft are teaming up for a 4 hour educational event to explore the latest state of the art of managing diabetes on the cloud followed by a hand-on workshop to help several families get up and running with the Nightscout kit. You can learn more and or register about the event here.
I will be attending the event to learn all I can and provide any technical support I can offer in the workshop though this is the first time I’ll be seeing the build myself. My goal is bring this event to Phoenix this year and I’m currently in conversations with JDRF, Microsoft and Nightscout leadership so stay tuned (I also got a soft commitment for the keynote from a highly prominent A-Lister that I promise any nerd will won’t want to miss wither you’ve been touched by T1D or not). I’d like to thank Ali Mazaheri and Katie Ryckman at Microsoft, Michelle Popoff at JDRF and Wes Ton of the Nightscout project for brining this event to Orange County and allowing me to participate. Last but not least, I’d like to thank Scott Hanselman for connecting me with the Nightscout project and teaching me that true community extends far beyond a platform or technology.
More to Come…
As you can tell, I’m pretty passionate about this project and you’ll be hearing from me a lot more (as well as hopefully seeing some commits from me on Github).
We didn’t ask for Type 1 Diabetes, and trust me, I’d give anything for God to take it back but I feel uniquely blessed to have the opportunity to be a part of this. As a father of the most amazing daughter in the world (who just happens to have T1D), being a Microsoft Azure MVP coupled with my interest in IoT gives me an amazing opportunity to apply my talents and interests for a greater good. Hopefully I can make a small difference.